- Research
- Open access
- Published:
Incidence, risk factors and outcomes of nosocomial infection in adult patients supported by extracorporeal membrane oxygenation: a systematic review and meta-analysis
Critical Care volume 28, Article number: 158 (2024)
Abstract
Background
An increasing number of patients requires extracorporeal membrane oxygenation (ECMO) for life support. This supportive modality is associated with nosocomial infections (NIs). This systematic review and meta-analysis aim to assess the incidence and risk factors of NIs in adult.
Methods
We searched PubMed, Scopus, Web of Science, and ProQuest databases up to 2022. The primary endpoint was incidence of NI. Secondary endpoints included time to infection, source of infection, ECMO duration, Intensive care and hospital length of stay (LOS), ECMO survival and overall survival. Incidence of NI was reported as pooled proportions and 95% confidence intervals (CIs), while dichotomous outcomes were presented as risk ratios (RR) as the effective index and 95% CIs using a random-effects model.
Results
Among the 4,733 adult patients who received ECMO support in the 30 included studies, 1,249 ECMO-related NIs per 1000 ECMO-days was observed. The pooled incidence of NIs across 18 studies involving 3424 patients was 26% (95% CI 14–38%).Ventilator-associated pneumonia (VAP) and bloodstream infections (BSI) were the most common NI sources. Infected patients had lower ECMO survival and overall survival rates compared to non-infected patients, with risk ratio values of 0.84 (95% CI 0.74–0.96, P = 0.01) and 0.80 (95% CI 0.71–0.90, P < 0.001), respectively.
Conclusion
Results showed that 16% and 20% lower of ECMO survival and overall survival in patients with NI than patients without NI, respectively. However, NI increased the risk of in-hospital mortality by 37% in infected patients compared with non-infected patients. In addition, this study identified the significant positive correlation between ECMO duration and ECMO-related NI.
Background
Extracorporeal membrane oxygenation (ECMO), also known as extracorporeal life support, is an advanced life support modality for critically-ill patients with severe but reversible cardiac and/or respiratory failure [1]. Despite improvements in both technology and management of ECMO, this technique is associated with specific risks and complications [2]. As consequences, many patients treated with ECMO face life-threatening complications such as bleeding, coagulopathy, thrombosis, infection, and stroke [3, 4].
Nosocomial infections (NI) are a common complication in patients treated with ECMO [5, 6]. Main sources of ECMO-related NI include bloodstream infections (BSIs), urinary tract infections (UTIs), surgical site infections (SSIs), and ventilator-associated pneumonia (VAP) [7, 8]. In addition to typical ECMO-related NI, specific ECMO-related infections, such as localized infections at peripheral cannulation insertion sites or mediastinitis in the setting of central cannulation also exists [9,10,11]. In studies examining different ECMO modalities, including (veno-venous) VV ECMO for respiratory failure and (veno-arterial) VA ECMO for cardiogenic shock, the infection risk was found to range from 8 to 64% [12,13,14,15]. Moreover, previous studies have suggested that NIs during ECMO may be related to some predisposing factors, including patients’ underlying condition, the severity of illness, and immunocompromised [16,17,18]. However, to date, there is no unified understanding of ECMO-related NI from diagnosis to treatment or prevention.
Significant heterogeneity may be expected from existing studies due to differences in case-mix, monocentric design of the performed studies, and inclusion of various ECMO modalities. This systematic review and meta-analysis aim to investigate the incidence of ECMO-related NIs as well as to examine ECMO survival, overall survival and the risk factors related to NI in published studies.
Methods
Study design
This systematic review and meta-analysis were performed according to predefined eligibility criteria, search strategies, criteria for study selection and methods for extracting data. It was performed according following the Preferred Reporting Items for Systematic review and Meta-Analysis Protocols (PRISMA-P) 2020 statement [19]. The predefined protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) database (CRD42023372412).
Search strategy and inclusion exclusion criteria
Electronic databases, including PubMed/MEDLINE, Scopus, Web of Science and ProQuest were searched from inception until 1st November 2022. English language publications reporting outcome and clinical characteristics of NI in adult patients receiving ECMO for more than 24 h were selected. To further identify articles for inclusion, all relevant studies and their citations list were examined. The full search strategy is available in Supplementary file 1, Table S1.
The PICOS (Population, Intervention, Comparison, Outcome, and Study type) mnemonic was used for synthesis in this meta-analysis to defined inclusion criteria [20]. Studies were eligible if they met all of the following inclusion criteria: (a) Population: adult (≥ 18 years) patients, male or female; (b) Intervention: supported by ECMO ≥ 24 h; (c) Comparison: compare NI patients with non-NI patients; (d) Outcomes: primary outcome indicators were the prevalence and incidence of NI, and secondary outcome indicators were ECMO survival, survival to hospital discharge, ECMO duration, ICU length of stay (LOS), hospital LOS, microorganism species causing ECMO-related NI, risk factors related to NI and related clinical characteristics of NI and (e) Study type: published retrospective or prospective cohort study. Studies were excluded if (a) studies enrolled patients who had been co-infected before receiving ECMO treatment; (b) studies without access to the full text, publication on animal experiments, review articles, letters-to-the-editor, editorial, case report and conference papers; (c) studies published in non- English languages.
A first screening was performed by title and abstract to identify seemingly related articles. A second screening was performed on selected article after complete assessment of the manuscripts. At each step, assessment was performed independently by two authors (A. AH and A.VA). Disagreement was resolved by discussion and if needed by adjudication by a third author. The final agreement between the three evaluating authors was assessed through Kendall's coefficient of agreement (r = 0.92; P < 0.001). Data were extracted from the included studies using a pre-designed form (Supplementary file 2, sheet 1). Moreover, the methodological quality of included manuscripts was assessed [21, 22].
Quality appraisal
The methodological quality of the included manuscripts was assessed using the JBI critical appraisal tool for cohort studies.. The tool evaluates cohort studies based on 11 criteria, with responses recorded as “Yes”, “No”, “Unclear”, or “Not Applicable”. After evaluating all components of the study, an overall rating was determined based on the number of “Yes” responses: good (≥ 8 yes), medium (5–7 yes), or poor (≤ 4 yes). In addition, the Cochrane Risk of Bias in Observational Studies of Exposures (ROBINS-E) tool was used to evaluate the risk of bias of the included studies [21, 22]. The ROBINS-E tool assesses 7 domains of bias: confounding, selection of participants into the study, classification of exposures, departures from intended exposures, missing data, measurement of outcomes and, selection of the reported result. Domains are classified as low risk of bias, high risk of bias, or unclear risk of bias [23].
Definition of NI and survival rates
ECMO-related NI was defined according to the Center for Disease Control and Prevention (CDC) as an infection occurring > 24 h after initiation and < 48 h after discontinuation of ECMO [24,25,26]. Various types of NIs include blood stream infection (BSI), respiratory tract infection (RTI), urinary tract infection (UTI), surgical site infection (SSI), cannula site infection (CSI), and ventilator-associated pneumonia (VAP) [27, 28]. The overall survival rate was defined as the percentage of patients with ECMO who survived to discharge from the hospital out of the total number of patients who received ECMO.
Primary and secondary outcomes
The primary outcome of this study was the incidence (NI per 1000 ECMO days) of different types of NI in adult patients receiving ECMO. The secondary outcomes included incidence (number of patients developing ≥ 1 episode of NI), time to infection, sources of infection, pathogens, duration of ECMO, ICU and hospital length of stay, ECMO and hospital survival rate.
Statistical analysis
Descriptive results were reported as percentages, mean ± standard deviation (SD) or median with interquartile range (IQR) calculated from the total number of patients in the analysis. GraphPad Prism 9© (GraphPad Software Inc., La Jolla, CA) and Excel program was used for and forest plots and graphs.
Incidence of NIs and its different types as primary outcomes were reported as pooled proportions and their 95% confidence intervals (CIs), while dichotomous outcomes were presented as pooled risk ratios (RR) and their 95% CIs. In addition, subgroups analysis was carried out based on countries. Due to methodologic variations and sample diversity across studies, the random-effects Linear Mixed Models (REML) was used to extract the pooled estimate. We applied the fixed effect model when the data were homogeneous.
Heterogeneity was assessed using the I-squared (I2) statistic, and significance results of the test and values > 50% for I2 indicated substantial heterogeneity and the corresponding p-values < 0.05 were also considered as significant [29]. In analyses with significant heterogeneity, a sensitivity analysis and meta-regression analysis were conducted to check the source of heterogeneity. In addition, we used the Galbraith plot to examine heterogeneity [30]. Risk of publication bias was evaluated by visual inspection of funnel plots, the Egger [31] and Begg [32] test were also conducted. Moreover, a nonparametric trim-and-fill method of assessing publication bias was conducted and if there was a publication bias the modified effect size was estimated after adjusting [33]. Finally, we assessed the effect of individual studies on ES, using cumulative analysis based on publication year. Statistical analyses were performed on Review Manager (RevMan) version 5, and STATA version 17 (Stata Corp; College Station; TX, USA). All tests were two-sided y and p-values lower than 0.05 was considered significant.
Results
Literature search and manuscript selection
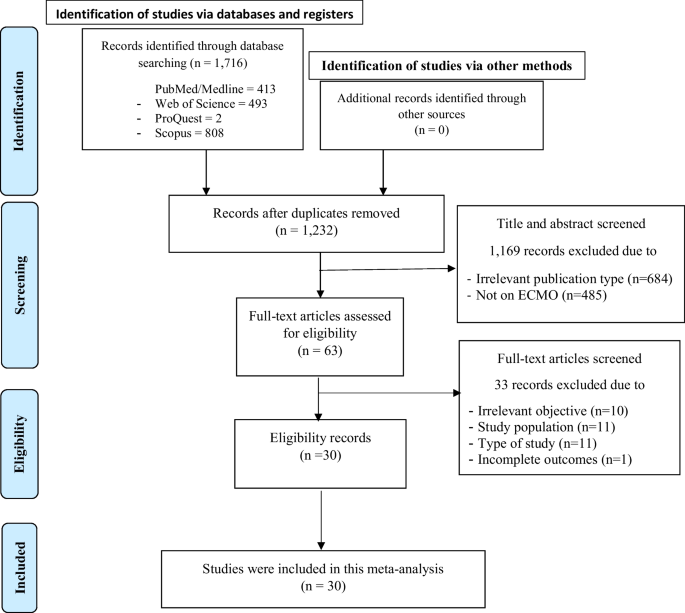
The search strategy included PubMed/Medline (n = 413), Web of Science (n = 493), ProQuest (n = 2) and Scopus (n = 808) databases resulting in 1,716 studies. After removing duplicates (n = 484) and irrelevant studies (n = 1169), 63 articles remained for full-text evaluation. Of these, 33 studies were excluded due to an inadequate study population (n = 11), inappropriate study design (n = 11) or lack of relevant outcome (n = 10) (Fig. 1). Details of the 33 excluded studies and the cause for their exclusion are available in Supplementary file 2, sheet 2.
Quality appraisal results
According to the results of quality assessment, most 24/30 (80%) studies had good quality [6, 8, 10, 12,13,14, 16, 34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50], and only 6/30 (20%) studies had moderate quality [17, 51,52,53,54,55] (Supplementary file 1, Table S2). In addition, 100% of included studies were classified as having low risk of bias based on Cochrane ROBINS-E tool (Supplementary file 1, Table S3–S4).
Characteristics of included studies.
Thirty studies with 4733 participants were included. Every one of these studies was of retrospective observational design. Of these participants, 65.4% (3097) were male and the median age was 50 (Range: 18–77). Among the included studies, only one was a multi-center retrospective study [55], while the rest were single-center retrospective studies. Main reason to initiate ECMO was need for cardiac support (63.1%, 2548), respiratory support (33.6%, n = 1356), and other causes for the remaining 3.3% (n = 135). Most of the studies included both VV ECMO and VA ECMO, four studies focusing only on VA ECMO [12, 16, 42, 51], and three studies on VV ECMO [37, 46, 54] (Tables 1 and 2).
Descriptive results
Clinical outcomes available in included studies are reported in Supplementary file 1, Table S5–S9. A comprehensive analysis of 30 studies involving 4733 adult patients on ECMO treatment revealed that there were 1249 ECMO-related NIs per 1000 ECMO-days. Males accounted for 60.93% of infected patients, with an average age of 53.17 ± 13.95 years. Hypertension was the most common underlying condition in both infected and non-infected patients (Supplementary file 1, Figure S1). Patients with NIs had significantly longer ECMO, ICU, and hospital stays (Supplementary file 1, Figure S1). The total incidence range of NIs was 4.1–85.4% with 2059 pathogens identified from 1,498 NI episodes in 1249 infected patients. The incidence of ECMO-related NI was 2.98–24.7% for BSI, 3.97–17% for SSI, 3.97–24.7% for RTI, 1.99–31% for UTI, 23.9–55.4% for VAP, and 7.1–11% for CSI. Gram-negative bacteria were identified as the most prevalent pathogens (48.6%), followed by Gram-positive bacteria and fungi. Acinetobacter baumannii, Pseudomonas aeruginosa, and Klebsiella pneumoniae were the most common Gram-negative bacteria, while Enterococcus spp., Coagulase-negative Staphylococcus, and Staphylococcus aureus were the predominant Gram-positive bacteria.
Risk factors for NI
Results showed that the MV duration, hospital LOS, ECMO mode (VV ECMO vs. VA ECMO), having underlying diseases (yes vs. no), mechanical complication, SOFA score, SAPS score, ECMO catheter colonization, age, duration of arterial catheter, acute renal failure, acute hepatic failure, body mass index (MBI), cardiopulmonary resuscitation (CPR) < 5 min and hemodialysis were significantly increased the risk of NI (Supplementary file 1, Figure S2B). According to pooled analysis in the current study, the cumulative odds ratio of ECMO duration to predict NI was 1.05 (95%CI 1.02–1.08, P < 0.001), with substantial significant heterogeneity between studies (I2 = 98.8%, P < 0.001) (Supplementary file 1, Figure S3).
Primary outcomes
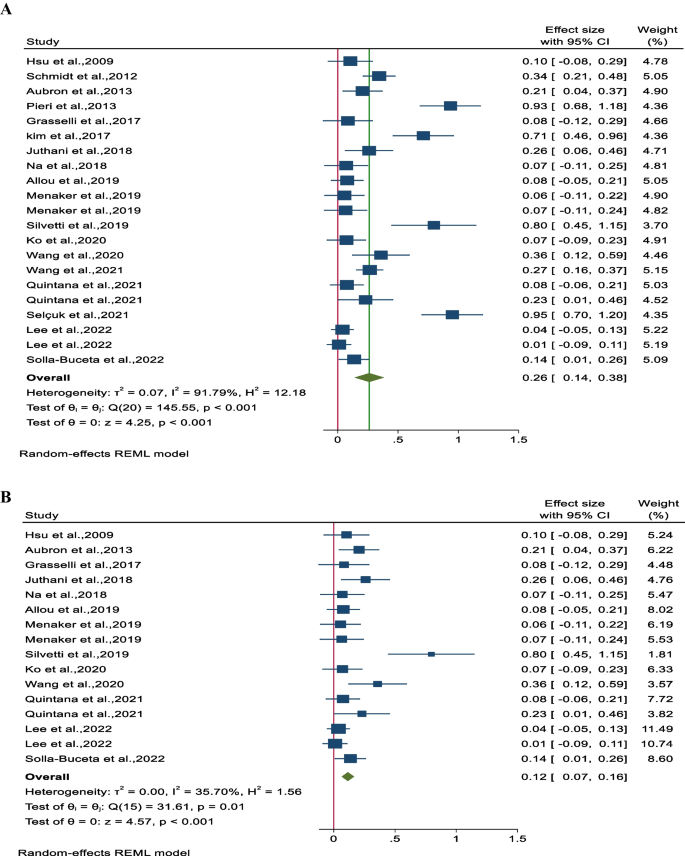
The pooled incidence rate of NIs, as reported in 18 studies involving 3,424 patients, was found to be 0.26 (95% CI 0.14–0.38, P < 0.001), indicating a statistically significant result. However, there was substantial heterogeneity observed between the studies (I2 = 91.8%, P < 0.001) (Fig. 2A). To address this heterogeneity, a sensitivity analysis was conducted where the study or studies causing the heterogeneity were excluded. Upon recalculating, the adjusted pooled incidence of NI (based on 13 studies and 2,761 patients) was determined to be 0.12 (95% CI 0.07–0.16, P < 0.001) with a mild heterogeneity (I2 = 35.7%, P = 0.01) (Fig. 2B).
Secondary outcomes
ECMO survival
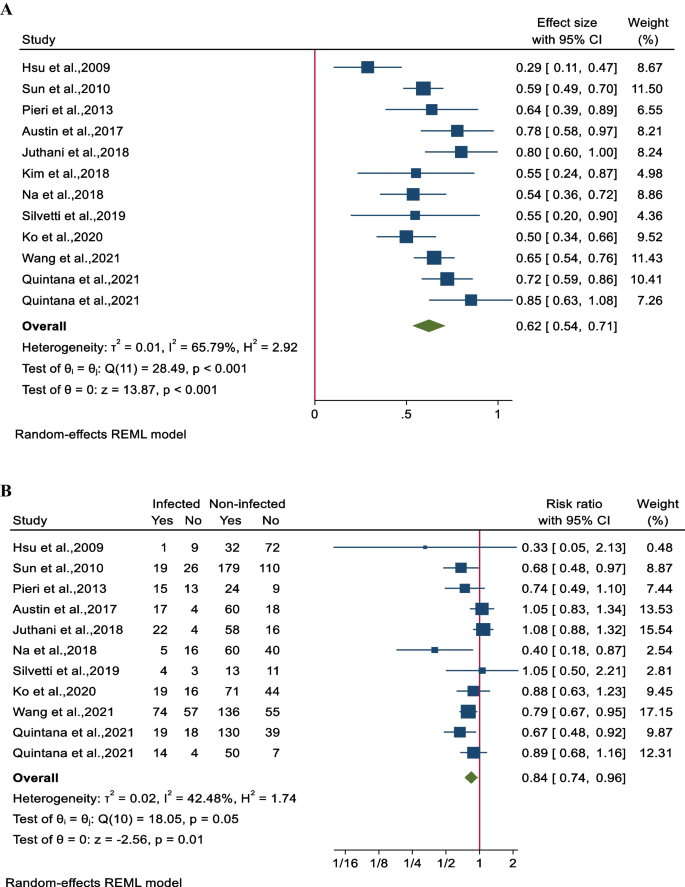
The survival rate of patients undergoing combined ECMO treatment was determined to be 62% (95% CI 54–70; 11 studies involving 1651 participants). Notably, there was substantial heterogeneity among the studies (I2 = 65.8%, P < 0.001 (Fig. 3A). The impact of nosocomial infections on ECMO survival was assessed in 10 studies involving 1613 patients. It was found that ECMO survival rates were significantly lower in patients with NIs, with a pooled risk ratio (RR) of 84% (95% CI 74–96%). A moderate level of heterogeneity was observed among the studies (I2 = 42.5%, P = 0.05) (Fig. 3B).
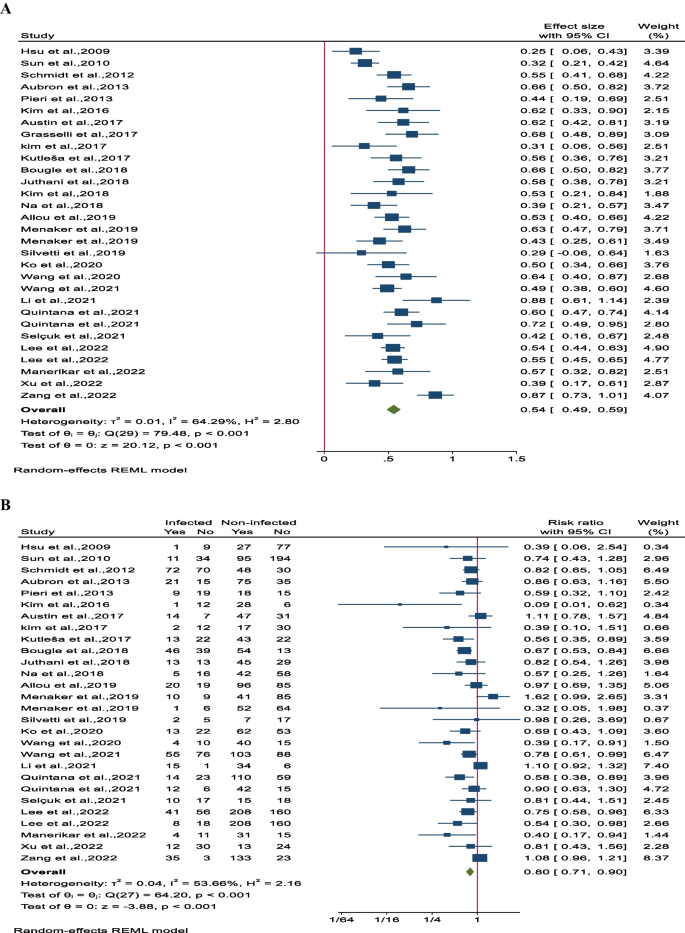
Overall survival
The overall survival rate was determined to be 54% (95% CI 49–59; 11 studies involving 1651 participants). Notably, there was significant heterogeneity observed among the studies (I2 = 64.5%, P < 0.001; Fig. 4A). Comparing the overall survival rates between the nosocomial infection (NI) group and control patients revealed a substantial difference, with the NI group showing a lower survival rate of 80% (95% CI 71–90; 24 studies involving 4205 patients). There was also notable heterogeneity among the studies (I2 = 53.7%, P < 0.001, Fig. 4B). Additionally, detailed subgroup analysis, sensitivity analysis, and assessment of publication bias can be found in Supplementary File 3, Figs. 1A–5D.
Time trend
Influence of NI on outcome was not affected by publication date (Supplementary file 1, Figure S4A). NI rate was however associated with the publication date (Supplementary file 1, Figure S4B). However, overall survival was lower among studies published from 2009 to 2013 (Supplementary file 1, Figure S5A–S5B).
Meta-regression
In order to explore the heterogeneity, a meta-regression analysis was conducted. Mortality was found to be linked to factors such as patients' severity of illness based on APACHE II scores, age, and VV ECMO, while ECMO survival was associated with nosocomial infections. The findings of the meta-regression analysis are presented in Supplementary File 1, Table S10. Additionally, a forest plot depicting the impact of these variables on the outcomes is included in Supplementary File 4, Figures S1–S19.
Discussion
This systematic review and meta-analysis aimed to assess the overall incidence of ECMO-related NIs and their impact on mortality, offering a comprehensive evaluation. Across 18 studies involving 3,424 patients, the pooled incidence of NIs was 26%. The time to the first NI ranged from 3 to 15.6 days after ECMO initiation, with a notable number of patients developing NIs beyond two weeks [16, 17, 44]. The incidence of NIs varied widely among studies, ranging from 4.1% to 85.4%. This variability could be attributed to factors like case mix, diagnostic criteria, reporting systems, antibiotic prophylaxis strategies, and center-specific effects [5, 56, 57].
The incidence of ECMO-related NIs and their impact on outcomes in patients supported by ECMO have been previously reported in literature. Studies have shown that the rate of infection can vary, with reports ranging from 8 to 46%. Previous reviews of the Extracorporeal Life Support Organization (ELSO) registry by Bizzarro et al. [58], and Vogel et al. [59], found rates of infection to be 11.7% and 10.2%, respectively, which is lower than the rates seen in our study. This discrepancy among studies may be attributed to differences in study populations, methodologies, variations in infection prevention practices, the emergence of new pathogens and antimicrobial resistance, as well as improvements in surveillance and reporting methods [60, 61].
Overall, 2059 pathogens were isolated from 1498 NI episodes in 1249 (26.4%) infected patients. Our findings identified VAP (33%), BSI (15%), and RTI (15%) as the most common ECMO-related NIs, primarily caused by GNB like Acinetobacter baumannii, Pseudomonas aeruginosa, and Klebsiella pneumoniae. Studies indicate VAP rates ranging from 10.7 to 54.5%, mainly attributed to GNB such as Pseudomonas aeruginosa, Klebsiella pneumoniae, and Acinetobacter species, and GPB like Staphylococcus aureus [8, 16, 17, 40, 47, 51]. BSI prevalence in adult ECMO patients ranges from 2.6 to 44.7%, with GBP, especially coagulase-negative staphylococci and Staphylococcus aureus, being the primary pathogens, followed by GNB (10–20%) such as Acinetobacter baumannii and Pseudomonas aeruginosa, and fungal infections like Candida spp. [13, 37, 39]. RTI rates vary from 1.1 to 32.1%, primarily caused by GNB like Klebsiella pneumoniae, Pseudomonas aeruginosa, and Haemophilus influenza [16, 51].
The study, consistent with the previous work by Li et al. [5], identified several risk factors for NIs in adult patients undergoing ECMO. These risk factors included the duration of MV, length of hospital stay, ECMO mode, underlying diseases, disease severity, ECMO catheter colonization, patient age, duration of arterial catheter placement, acute renal failure, acute hepatic failure, BMI, ECPR exceeding 5 min, hemodialysis, and mechanical complications. Patients supported by VV ECMO exhibited a higher susceptibility to developing Nosocomial Infections (NIs) compared to those on VA ECMO [14, 41, 47]. Despite this, the VA ECMO modality is recognized for its increased complexity, entailing higher risks of vascular trauma, systemic embolization, and ischemia [62]. The exact reason behind the heightened NI risk in VV ECMO patients remains somewhat ambiguous. This elevated risk may be linked to the prolonged ECMO treatment and duration of ventilator support in VV ECMO patients [14, 41]. Additionally, the longer duration of VV ECMO in lung transplant recipients inherently exposes them to an extended period of susceptibility to NIs, potentially leading to skewed infection rates and outcomes when contrasted with heart transplant patients supported by VA ECMO with shorter durations of support. The study highlights a significant association between NIs and adverse outcomes in adult ECMO patients, resulting in a relative risk reduction of 16% in ECMO survival rates and 20% in overall survival rates. Moreover, NIs were found to elevate the relative risk of hospital mortality, particularly in cases of prolonged ECMO duration, which showed a potential four-fold increase in NI risk [34, 37, 38, 42, 45, 47, 52, 55].This heightened risk can be attributed to the critical condition of patients on long-term ECMO, prolonged exposure to risks, and the intensity of invasive care. Time-dependent bias is a critical consideration in studies involving ECMO duration and nosocomial infections. In the context of ECMO, the duration of ECMO support can act both as a risk factor for developing infections and as a consequence of infection occurrence. Prolonged ECMO duration has been associated with an increased risk of nosocomial infections due to factors such as prolonged exposure to invasive devices, prolonged hospitalization, and compromised immune function [63]. Longer ECMO duration not only increases the likelihood of acquiring infections but can also be a consequence of infections that prolong the need for ECMO support. This bidirectional relationship underscores the complexity of managing infections in ECMO patients and emphasizes the need for vigilant monitoring, infection prevention strategies, and timely interventions to mitigate the risks associated with prolonged ECMO support.
The observed increase in NI rates in more recent studies [45,46,47,48], despite older studies showing lower survival rates is indeed a noteworthy finding [13, 14, 16]. This apparent discrepancy does not necessarily negate the conclusion that NIs can impact mortality in ECMO patients. Instead, it may reflect improved surveillance, detection, and reporting of NIs over time. One plausible explanation for this occurrence could be advancements in critical care practices and infection control measures over time. With improvements in healthcare protocols, including enhanced sepsis management, antimicrobial stewardship, and ECMO circuit technology, it is possible that while NI rates have risen in recent years, overall survival rates have improved due to better management of infections. Moreover, the evolving landscape of ECMO therapy, including patient selection criteria, cannulation techniques, and anticoagulation strategies, may have influenced both NI rates and patient outcomes over time. The study could be useful for clinicians and researchers regarding infection risk factors in ECMO patients. Further studies aiming at identifying high-risk patients are needed so that clinicians and researchers can pinpoint high-risk patients for tailored monitoring and interventions.
This study has several limitations that should be considered. Firstly, the retrospective and single-center nature of most included studies, along with small sample sizes, limits data availability on confounding factors and the establishment of appropriate exposure and comparison groups. Secondly, there was significant heterogeneity due to variations in case mix, nosocomial infection rates, and management practices across different centers. Thirdly, a notable limitation is the inadequate consideration of time dependency of nosocomial infections in most studies, potentially leading to misleading associations between ECMO/ICU duration and infection outcomes. Lastly, the potential impact of changes in sepsis definitions and management practices over the years on the identification of BSI in ECMO patients is a critical consideration. These evolving standards may introduce variability in how infections are identified and managed, which could affect the study's outcomes. To address these limitations, we have conducted sensitivity analyses to mitigate potential biases arising from these changes, ensuring the robustness of our results. These limitations highlight the need for future research to address these gaps and improve our understanding of the impact of NIs on patient outcomes.
Conclusion
This study highlights a heightened risk of NIs, particularly Ventilator-VAP, BSI, and RTI, in patients undergoing ECMO for refractory respiratory or cardiogenic failure. The pooled analysis revealed a 26% incidence rate per 1000 ECMO-days of NIs in adult ECMO patients. Our findings indicate a 16% and 20% lower ECMO survival and overall survival, respectively, in patients with NIs compared to those without. The dynamic nature of ECMO therapy, encompassing evolving patient selection criteria, cannulation techniques, and anticoagulation strategies, may have impacted both NI rates and patient outcomes. Further research is warranted to delve deeper into assessing the risk of nosocomial infections while considering time-dependent confounders, evaluating the efficacy of prevention strategies, and understanding their impact on both infection rates and outcomes.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- ECMO:
-
Extracorporeal membrane oxygenation
- NIs:
-
Nosocomial infections
- BSIs:
-
Bloodstream infections
- UTIs:
-
Urinary tract infections
- SSIs:
-
Surgical site infections
- VAP:
-
Ventilator-associated pneumonia
- CSI:
-
Cannula site infection
- VA ECMO:
-
Venoarterial extracorporeal membrane oxygenation
- VV ECMO:
-
Venovenous extracorporeal membrane oxygenation
- LOS:
-
Length of stay
- CIs:
-
Confidence intervals
- RR:
-
Risk ratios
- REML:
-
Linear Mixed Models
References
Ventetuolo CE, Muratore CS. Extracorporeal life support in critically ill adults. Am J Respir Crit Care Med. 2014;190(5):497–508. https://doi.org/10.1164/rccm.201404-0736CI.
Coco LV, Lorusso R, Raffa GM, Malvindi PG, Pilato M, Martucci G, et al. Clinical complications during veno-arterial extracorporeal membrane oxigenation in post-cardiotomy and non post-cardiotomy shock: still the achille’s heel. J Thorac Dis. 2018;10(12):6993–7004. https://doi.org/10.21037/jtd.2018.11.103.
Kim JH, Pieri M, Landoni G, Scandroglio AM, Calabrò MG, Fominskiy E, et al. Venovenous ECMO treatment, outcomes, and complications in adults according to large case series: a systematic review. Int J Artif Organs. 2020;44(7):481–8. https://doi.org/10.1177/0391398820975408.
Zangrillo A, Landoni G, Biondi-Zoccai G, Greco M, Greco T, Frati G, et al. A meta-analysis of complications and mortality of extracorporeal membrane oxygenation. Crit Care Resusc. 2013;15(3):172–8.
Li X, Wang L, Wang H, Hou X. Outcome and clinical characteristics of nosocomial infection in adult patients undergoing extracorporeal membrane oxygenation: a systematic review and meta-analysis. Front Public Health. 2022;10: 857873. https://doi.org/10.3389/fpubh.2022.857873.
Li ZJ, Zhang DF, Zhang WH. Analysis of nosocomial infection and risk factors in patients with ECMO treatment. Infect Drug Resist. 2021;14:2403–10. https://doi.org/10.2147/IDR.S306209.
Wang J, Christensen C, Siddique A, Merritt H, Cawcutt K. Characteristics of venous–venous extracorporeal membrane oxygenation related bloodstream infections. J Card Surg. 2022;37(5):1431–4. https://doi.org/10.1111/jocs.16361.
Aubron C, Cheng AC, Pilcher D, Leong T, Magrin G, Cooper DJ, et al. Infections acquired by adults who receive extracorporeal membrane oxygenation: risk factors and outcome. Infect Control Hosp Epidemiol. 2013;34(1):24–30. https://doi.org/10.1086/668439.
Thomas G, Hraiech S, Cassir N, Lehingue S, Rambaud R, Wiramus S, et al. Venovenous extracorporeal membrane oxygenation devices-related colonisations and infections. Ann Intensive Care. 2017. https://doi.org/10.1186/s13613-017-0335-9.
Allou N, Lo Pinto H, Persichini R, Bouchet B, Braunberger E, Lugagne N, et al. Cannula-related infection in patients supported by peripheral ECMO: clinical and microbiological characteristics. ASAIO J. 2019;65(2):180–6. https://doi.org/10.1097/MAT.0000000000000771.
Bull T, Corley A, Lye I, Spooner AJ, Fraser JF. Cannula and circuit management in peripheral extracorporeal membrane oxygenation: an international survey of 45 countries. PLoS ONE. 2019;14(12): e0227248. https://doi.org/10.1371/journal.pone.0227248.
Silvetti S, Ranucci M, Pistuddi V, Isgro G, Ballotta A, Ferraris L, et al. Bloodstream infections during post-cardiotomy extracorporeal membrane oxygenation: incidence, risk factors, and outcomes. Int J Artif Organs. 2019;42(6):299–306. https://doi.org/10.1177/0391398818817325.
Hsu MS, Chiu KM, Huang YT, Kao KL, Chu SH, Liao CH. Risk factors for nosocomial infection during extracorporeal membrane oxygenation. J Hosp Infect. 2009;73(3):210–6. https://doi.org/10.1016/j.jhin.2009.07.016.
Sun HY, Ko WJ, Tsai PR, Sun CC, Chang YY, Lee CW, et al. Infections occurring during extracorporeal membrane oxygenation use in adult patients. J Thorac Cardiovasc Surg. 2010;140(5):1125-1132.e1122. https://doi.org/10.1016/j.jtcvs.2010.07.017.
O’Neill JM, Schutze GE, Heulitt MJ, Simpson PM, Taylor BJ. Nosocomial infections during extracorporeal membrane oxygenation. Intensive Care Med. 2001;27(8):1247–53. https://doi.org/10.1007/s001340101029.
Schmidt M, Brechot N, Hariri S, Guiguet M, Luyt CE, Makri R, et al. Nosocomial infections in adult cardiogenic shock patients supported by venoarterial extracorporeal membrane oxygenation. Clin Infect Dis. 2012;55(12):1633–41. https://doi.org/10.1093/cid/cis783.
Grasselli G, Scaravilli V, Di Bella S, Biffi S, Bombino M, Patroniti N, et al. Nosocomial infections during extracorporeal membrane oxygenation: incidence, etiology, and impact on patients’ outcome. Crit Care Med. 2017;45(10):1726–33. https://doi.org/10.1097/CCM.0000000000002652.
Biffi S, Di Bella S, Scaravilli V, Peri AM, Grasselli G, Alagna L, et al. Infections during extracorporeal membrane oxygenation: epidemiology, risk factors, pathogenesis and prevention. Int J Antimicrob Agents. 2017;50(1):9–16. https://doi.org/10.1016/j.ijantimicag.2017.02.025.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71. https://doi.org/10.1136/bmj.n71.
Cumpston MS, McKenzie JE, Thomas J, Brennan SE. The use of ‘PICO for synthesis’ and methods for synthesis without meta-analysis: protocol for a survey of current practice in systematic reviews of health interventions. F1000Research. 2020. https://doi.org/10.12688/f1000research.24469.2.
Morgan RL, Thayer KA, Santesso N, Holloway AC, Blain R, Eftim SE, et al. Evaluation of the risk of bias in non-randomized studies of interventions (ROBINS-I) and the 'target experiment’ concept in studies of exposures: rationale and preliminary instrument development. Environ Int. 2018;120:382–7. https://doi.org/10.1016/j.envint.2018.08.018.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343: d5928. https://doi.org/10.1136/bmj.d5928.
Wang WW, Zhou QX, Ma L, Feng SH, Yang ZR, Sun F, et al. Introduction of a tool to assess risk of bias in non-randomized studies-of environmental exposure (ROBINS-E). Zhonghua Liu Xing Bing Xue Za Zhi. 2022;43(1):98–104. https://doi.org/10.3760/cma.j.cn112338-20201112-01324.
Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988;16(3):128–40. https://doi.org/10.1016/0196-6553(88)90053-3.
Centers for Disease Control and Prevention (CDC). CDC/NHSN surveillance definitions for specific types of infections. 2018; (17): 1–30.
Mornese Pinna S, Sousa Casasnovas I, Olmedo M, Machado M, Juàrez Fernández M, Devesa-Cordero C, et al. Nosocomial infections in adult patients supported by extracorporeal membrane oxygenation in a cardiac intensive care unit. Microorganisms. 2023. https://doi.org/10.3390/microorganisms11041079.
Haque M, Sartelli M, McKimm J, Abu BM. Health care-associated infections—an overview. Infect Drug Resist. 2018;11:2321–33. https://doi.org/10.2147/idr.S177247.
Control CfD, Prevention. Pneumonia (ventilator-associated [VAP] and non-ventilator-associated pneumonia [PNEU]) event. Device-associated Module PNEU/VAP. 2015.
Cumpston MS, McKenzie JE, Welch VA, Brennan SE. Strengthening systematic reviews in public health: guidance in the cochrane handbook for systematic reviews of interventions. J Public Health. 2022. https://doi.org/10.1093/pubmed/fdac036.
Wang D, Mou ZY, Zhai JX, Zong HX, Zhao XD. Application of Stata software to test heterogeneity in meta-analysis method. Zhonghua Liu Xing Bing Xue Za Zhi. 2008;29(7):726–9.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. https://doi.org/10.1136/bmj.315.7109.629.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101.
Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–63. https://doi.org/10.1111/j.0006-341x.2000.00455.x.
Pieri M, Agracheva N, Fumagalli L, Greco T, De Bonis M, Calabrese MC, et al. Infections occurring in adult patients receiving mechanical circulatory support: the two-year experience of an Italian national referral tertiary care center. Med Intensiva. 2013;37(7):468–75. https://doi.org/10.1016/j.medin.2012.08.009.
Kim DW, Yeo HJ, Yoon SH, Lee SE, Lee SJ, Cho WH, et al. Impact of bloodstream infections on catheter colonization during extracorporeal membrane oxygenation. J Artif Organs. 2016;19(2):128–33. https://doi.org/10.1007/s10047-015-0882-5.
Kim GS, Lee KS, Park CK, Kang SK, Kim DW, Oh SG, et al. Nosocomial infection in adult patients undergoing veno-arterial extracorporeal membrane oxygenation. J Korean Med Sci. 2017;32(4):593–8. https://doi.org/10.3346/jkms.2017.32.4.593.
Kutleša M, Santini M, Krajinović V, Papić N, Novokmet A, Josipović Mraović R, et al. Nosocomial blood stream infections in patients treated with venovenous extracorporeal membrane oxygenation for acute respiratory distress syndrome. Minerva Anestesiol. 2017;83(5):493–501. https://doi.org/10.23736/S0375-9393.17.11659-7.
Sun G, Li B, Lan H, Wang J, Lu L, Feng X, et al. Risk factors for nosocomial infections in patients receiving extracorporeal membrane oxygenation supportive therapy. Med Clin. 2017;149(10):423–8. https://doi.org/10.1016/j.medcli.2017.03.038.
Menaker J, Galvagno S, Rabinowitz R, Penchev V, Hollis A, Kon Z, et al. Epidemiology of blood stream infection in adult extracorporeal membrane oxygenation patients: a cohort study. Heart Lung. 2019;48(3):236–9. https://doi.org/10.1016/j.hrtlng.2019.01.004.
Ko RE, Huh K, Kim DH, Na SJ, Chung CR, Cho YH, et al. Nosocomial infections in in-hospital cardiac arrest patients who undergo extracorporeal cardiopulmonary resuscitation. PLoS ONE. 2020. https://doi.org/10.1371/journal.pone.0243838.
Wang J, Huang J, Hu W, Cai X, Hu W, Zhu Y. Risk factors and prognosis of nosocomial pneumonia in patients undergoing extracorporeal membrane oxygenation: a retrospective study. J Int Med Res. 2020. https://doi.org/10.1177/0300060520964701.
Wang J, Wang L, Jia M, Du Z, Hou X. Extracorporeal membrane oxygenation-related nosocomial infection after cardiac surgery in adult patients. Braz J Cardiovasc Surg. 2021;36(6):743–51. https://doi.org/10.21470/1678-9741-2020-0068.
Quintana MT, Mazzeffi M, Galvagno SM, Herrera D, Boyajian GP, Hays NM, et al. A retrospective study of infection in patients requiring extracorporeal membrane oxygenation support. Ann Thorac Surg. 2021;112(4):1168–75. https://doi.org/10.1016/j.athoracsur.2020.12.012.
Selçuk ÜN, Sargın M, Baştopçu M, Mete EMT, Erdoğan SB, Öcalmaz Ş, et al. Microbiological spectrum of nosocomial ECMO infections in a tertiary care center. Braz J Cardiovasc Surg. 2021;36(3):338–45. https://doi.org/10.21470/1678-9741-2020-0077.
Lee EH, Lee KH, Lee SJ, Kim J, Baek YJ, Ahn JY, et al. Clinical and microbiological characteristics of and risk factors for bloodstream infections among patients with extracorporeal membrane oxygenation: a single-center retrospective cohort study. Sci Rep. 2022. https://doi.org/10.1038/s41598-022-19405-z.
Manerikar A, Watanabe S, Kandula V, Karim A, Thakkar S, Saine M, et al. Indwelling central venous catheters drive bloodstream infection during veno-venous extracorporeal membrane oxygenation support. ASAIO J. 2022;68(6):859–64. https://doi.org/10.1097/MAT.0000000000001575.
Xu W, Fu Y, Yao Y, Zhou J, Zhou H. Nosocomial infections in nonsurgical patients undergoing extracorporeal membrane oxygenation: a retrospective analysis in a Chinese hospital. Infect Drug Resist. 2022;15:4117–26. https://doi.org/10.2147/IDR.S372913.
Zang F, Zhang X, Liu J, Li S, Zhang Y, Li Z. Hospital expenses of nosocomial infection associated with extracorporeal membrane oxygenation in China: a retrospective cohort study. Ann Palliat Med. 2022;11(2):431–41. https://doi.org/10.21037/apm-21-1825.
Austin DE, Kerr SJ, Al-Soufi S, Connellan M, Spratt P, Goeman E, et al. Nosocomial infections acquired by patients treated with extracorporeal membrane oxygenation. Crit Care Resusc. 2017;19:68–75.
Li B, Sun G, Cheng Z, Mei C, Liao X, Li J, et al. Analysis of nosocomial infections in post-cardiac surgery extracorporeal membrane oxygenation support therapy. Heart Surg Forum. 2018;21(5):E387–91. https://doi.org/10.1532/hsf.1789.
Bougle A, Bombled C, Margetis D, Lebreton G, Vidal C, Coroir M, et al. Ventilator-associated pneumonia in patients assisted by veno-arterial extracorporeal membrane oxygenation support: epidemiology and risk factors of treatment failure. PLoS ONE. 2018. https://doi.org/10.1371/journal.pone.0194976.
Juthani BK, Macfarlan J, Wu J, Misselbeck TS. Incidence of nosocomial infections in adult patients undergoing extracorporeal membrane oxygenation. Heart Lung. 2018;47(6):626–30. https://doi.org/10.1016/j.hrtlng.2018.07.004.
Kim DW, Cho HJ, Kim GS, Song SY, Na KJ, Oh SG, et al. Predictive value of procalcitonin for infection and survival in adult cardiogenic shock patients treated with extracorporeal membrane oxygenation. Chonnam Med J. 2018;54(1):48–54. https://doi.org/10.4068/cmj.2018.54.1.48.
Na SJ, Chung CR, Choi HJ, Cho YH, Yang JH, Suh GY, et al. Blood stream infection in patients on venovenous extracorporeal membrane oxygenation for respiratory failure. Infect Control Hosp Epidemiol. 2018;39(7):871–4. https://doi.org/10.1017/ice.2018.90.
Solla-Buceta M, Gonzalez-Vilchez F, Almenar-Bonet L, Lambert-Rodriguez JL, Segovia-Cubero J, Gonzalez-Costello J, et al. Infectious complications associated with short-term mechanical circulatory support in urgent heart transplant candidates. Rev Esp Cardiol. 2022;75(2):141–9. https://doi.org/10.1016/j.rec.2020.11.019.
Seidelman JL, Lewis SS, Huslage K, Strittholt N, Vereen S, Sova C, et al. To be a CLABSI or not to be a CLABSI-that is the question: the epidemiology of BSI in a large ECMO population. Infect Control Hosp Epidemiol. 2018;39(3):362–5. https://doi.org/10.1017/ice.2017.320.
Fu KX, MacLaren G. Infectious complications of postcardiotomy extracorporeal membrane oxygenation. Pediatr Critic Care Med. 2020;21(11):1019–20. https://doi.org/10.1097/pcc.0000000000002447.
Bizzarro MJ, Conrad SA, Kaufman DA, Rycus P. Infections acquired during extracorporeal membrane oxygenation in neonates, children, and adults. Pediatr Critic Care Med. 2011;12(3):277–81. https://doi.org/10.1097/PCC.0b013e3181e28894.
Vogel AM, Lew DF, Kao LS, Lally KP. Defining risk for infectious complications on extracorporeal life support. J Pediatr Surg. 2011;46(12):2260–4. https://doi.org/10.1016/j.jpedsurg.2011.09.013.
Peña-López Y, Machado MC, Rello J. Infection in ECMO patients: changes in epidemiology, diagnosis and prevention. Anaesth Critic Care Pain Med. 2024;43(1): 101319. https://doi.org/10.1016/j.accpm.2023.101319.
Peitz GJ, Murry DJ. The influence of extracorporeal membrane oxygenation on antibiotic pharmacokinetics. Antibiotics. 2023;12(3):500.
Maclaren G, Butt W. Extracorporeal membrane oxygenation and sepsis. Crit Care Resusc. 2007;9(1):76–80.
MacLaren G, Schlapbach LJ, Aiken AM. Nosocomial infections during extracorporeal membrane oxygenation in neonatal, pediatric, and adult patients: a comprehensive narrative review. Pediatr Critic Care Med J Soc Critic Care Med World Federation Pediatr Intensiv Critic Care Soc. 2020;21(3):283–90. https://doi.org/10.1097/pcc.0000000000002190.
Acknowledgements
Thanks to guidance and advice from the “Clinical Research Development Unit" of Baqiyatallah Hospital.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
A.AH, A.VA and M.D contributed to the conception and design of the study. A.AH, A.VA and A.SI performed the title and abstract screening. A.SI, I.FH and E.A performed the data extraction. A.SI and M.D organized the data and created the characteristic tables. A.VA and A.AH performed the data analysis. A.AH, I.FH and A.SI wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The predefined protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) database (CRD42023372412).
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest to disclose related to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ait Hssain, A., Vahedian-Azimi, A., Ibrahim, A.S. et al. Incidence, risk factors and outcomes of nosocomial infection in adult patients supported by extracorporeal membrane oxygenation: a systematic review and meta-analysis. Crit Care 28, 158 (2024). https://doi.org/10.1186/s13054-024-04946-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-024-04946-8